Artificial Skin — Ioannis V. Yannas (1982)
[SIRENS]
NARRATOR: Each year, fire injures more than 100,000 people nationwide. Burn victims lose protective skin and can die from fluid loss and infection. But there is hope-- artificial skin developed at Massachusetts Institute of Technology and Massachusetts General Hospital, Shriners Burns institute.
BURKE: The major threat to a patient with a very large burn injury is infection in the area of a wound that has not been closed with skin. And the sooner you can close the wound with the skin or a skin substitute-- an artificial skin in this case-- the more likely it is to avoid infection and therefore all of the problems of infection. So we are very anxious to move quickly in these cases to excise all of the tissue that's been killed and to close the wound. And artificial skin allows us to do that very much more rapidly than if we had to wait until regeneration of some of the patient's own skin.
The artificial skin extends from here to here. The skin here, the conventional drafting is a little more irregular, slightly more pigmented than one would expect at this part of the body, and not quite as resilient as the artificial material.
NARRATOR: 3,500 years ago, Egyptians tried meat and honey to treat wounds. Today, after 11 years of research, Doctor Burke of Massachusetts General Hospital and Professor Yannas at Massachusetts Institute of Technology have developed artificial skin that works.
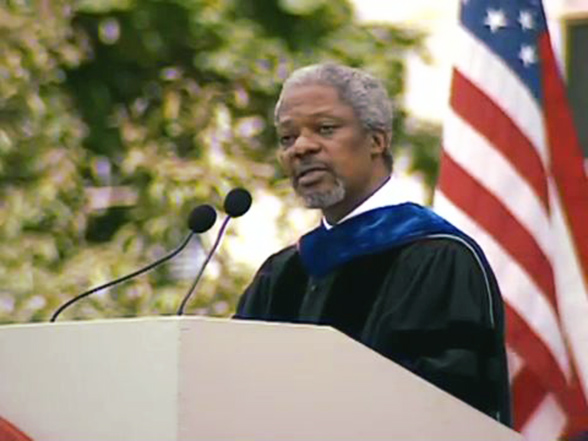
YANNAS: Our 11-year research effort can be looked at in two ways. First, we have addressed the urgent surgical problem of treating the massively burn patient and keeping that patient alive. Secondly, we have treated skin loss in somewhat of a basic way. Rather than constructing an organ and putting it in the patient, we have managed to construct a biological mold, because that's what the artificial skin is. This biological mold is used by the patient to regrow or rebuild the skin that was lost in injury.
NARRATOR: This is a unique process. A man-made material activates the body to heal itself, allowing complete restoration of lost skin. After years of animal testing, they found the right ingredients-- a blend of collagen and a polysaccharide.
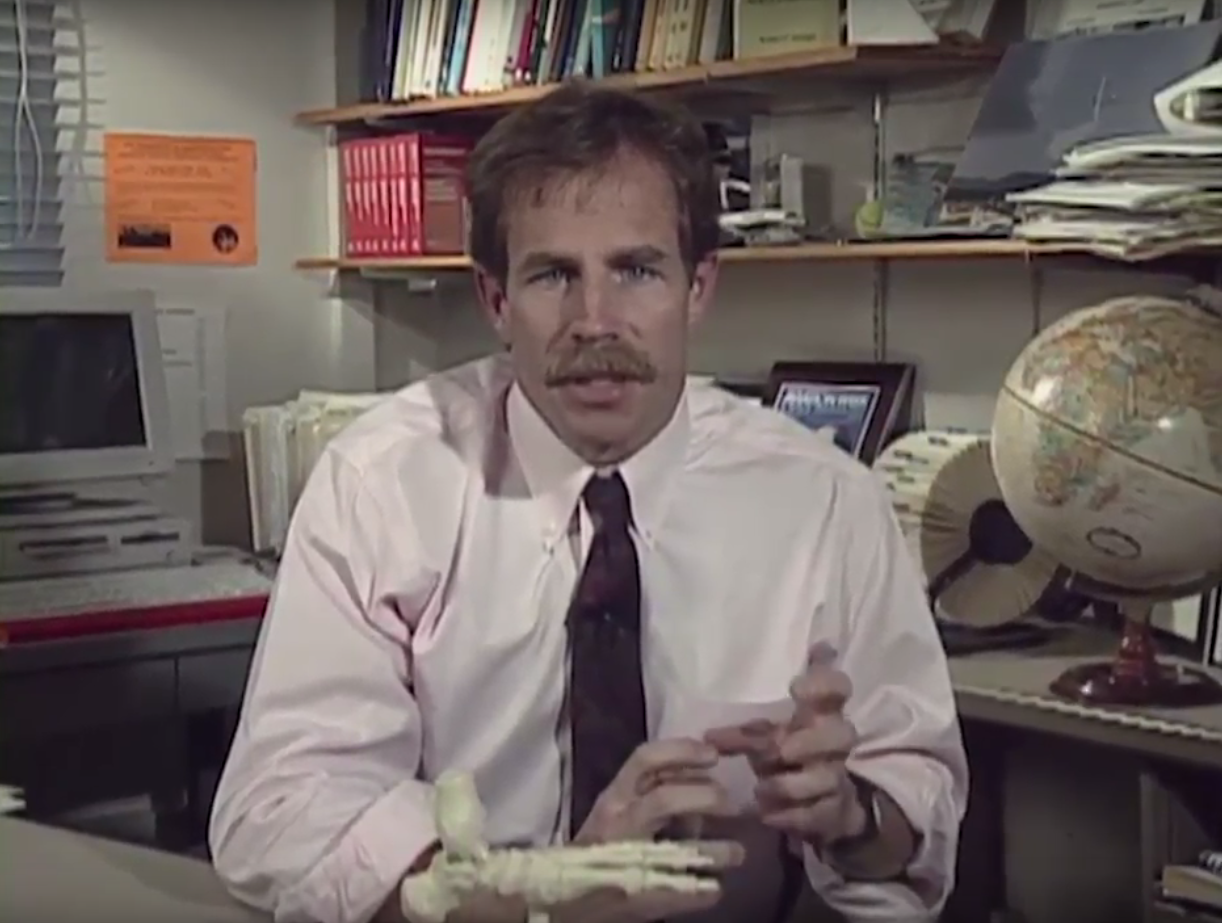
YANNAS: This material is collagen, fiber protein which is one of the basic ingredients of our artificial skin. Collagen fibers reinforce mechanically many of our tissues-- tendon, ligament, and skin. Our development of the artificial skin has in some ways followed the design of our own natural skin, which is made up of two layers.
The outer layer is the epidermis, which is a moisture seal and a bacteria seal. And in the artificial skin, this top layer plays the same role. The bottom layer is a mechanical seal, pretty much as the dermis, the inner layer of our own natural skin, acts as a mechanical seal.
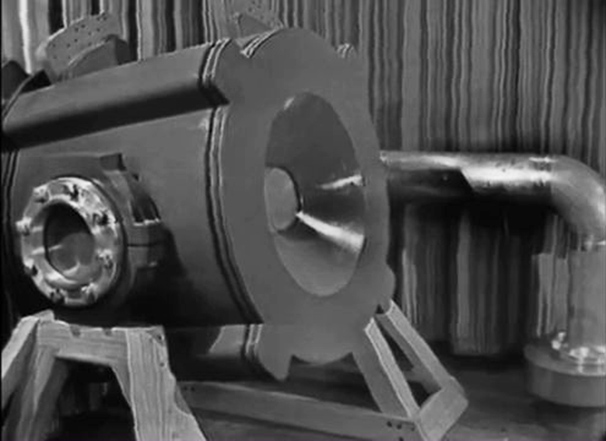
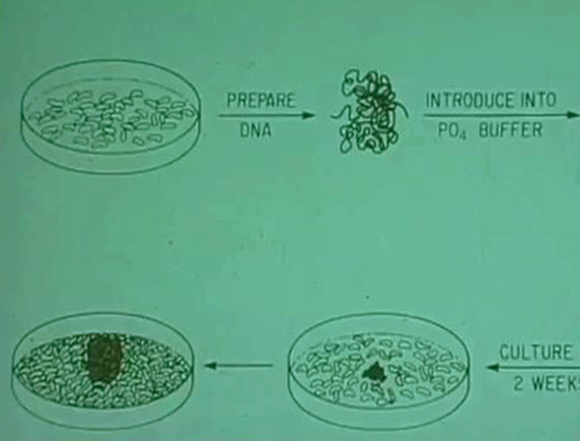
NARRATOR: Here's the collagen polysaccharide mixture. The mix is freeze dried and then heated to chemically bind the components. Freeze drying develops the porous structure of the mixture. Finally, the collagen is ready for a silicone layer. Silicone makes the artificial skin suturable, controls the rate of moisture release, and it keeps out bacteria.
YANNAS: This is a segment of the completed artificial skin. This is the form in which this material is handed over to the surgeon for grafting of wounds. You can see that it can be stretched, it can be sutured, it is flexible and drapes well over curved surfaces, and it is somewhat transparent.
NARRATOR: Sutured. Skin cells grow through the collagen, and then the body eliminates the collagen. Silicone is peeled off. Finally, epidermis is surgically applied. Recent research on animals shows that by seeding basal cells on the artificial skin, both layers of skin grow over the wound. 11 years of research has paid off. Artificial skin has been successfully used on 35 severely burned people. Used experimentally until now, it will soon be widely available.