Women of MIT: Celebrating Science and Engineering Breakthroughs (Session I)
SIVE: I'd like to welcome you to this first afternoon of this historic symposium. Historic not only because it brings together people who have considered societal issues and considered policy issues, and have changed policy to move women to where they should be as intellectual leaders. But also because it brings together leaders in the fields of science and engineering who are some of our most eminent faculty here at MIT and who have agreed to respond to our invitation and tell you about the truly extraordinary work that they're doing. And it's my honor to introduce three of those to you this afternoon.
The first is Susan Lindquist. Professor Lindquist received her PhD in biology from Harvard University and became a member of the faculty at the University of Chicago later, prior to coming to MIT in 2001. She came to MIT as Director of the Whitehead Institute for Biomedical Research, and continues to be a Member of the Whitehead Institute and a member of the biology department, Professor of Biology at MIT. She is a Howard Hughes Medical Institute investigator whose work addresses fundamental mechanisms regulating protein folding. And as she will tell us, this has profoundly changed our understanding of normal and pathologic conditions.
Her list of honors is extraordinary as her research. She was elected to the American Academy of Arts and Sciences in 1997, the National Academy of Sciences also in '97, and the Institute of Medicine in 2006. In a single stunning month last year, Professor Lindquist received our nation's highest honor, the National Medal of Science, as well as the Max Delbruck Medal, and the Mendel Medal.
The title of her talk is-- "Using Simple Cells to Attack Complex Diseases." Professor Lindquist.
LINDQUIST: Hi there. Thank you. I'm really honored to be here.
Chuck mentioned the double helix today. I'm going to start out by reminding you that the genomes that we all have are made of linear DNA, long linear strings of information. And what they do primarily is code for proteins. So just about everything that makes you you is done by a protein.
And when proteins are first decoded from the linear information of the DNA, they are also linear. They are long strings of amino acids. But they do nothing in those shapes. They have to fold into some very, very complicated shapes, like this. And this.
And the crazy thing is that they have to do that in an absolutely ridiculous environment. They have to do that inside of a living cell where the concentration of other proteins is amazingly high. So if you look at those proteins in their context inside the cell, you can see how incredibly crowded it is. And what you're not really seeing here with this image is that not only is it crowded, but the cells are experiencing a tremendous amount of kinetic energy. So the proteins are moving around like crazy and constantly bumping into each other. So that when you think about proteins going about their business inside of a living cell, it's not like Fred Astaire and Ginger Rogers. It's much more like the characters in a Marx brothers movie, where chaos is poised on the precipice of disaster.
And so in the full protein folding world we call that going off-pathway. And it's happening all the time in living cells. And it's responsible for some of mankind's most devastating diseases. Including these neurodegenerative diseases: frontotemporal dementia and ALS, Parkinson's, dementia with Lewy bodies, multiple systems atrophy, Huntington's, Alzheimer's, prion diseases. These are all characterized by globs of misfolded proteins. So you might have heard of plaques, amyloid plaques, in the brains of Alzheimer's disease victims. Those plaques are plaques of misfolded protein.
And so this is, it turns out, this protein folding problem is as ancient as life itself. Cells are built to be so incredibly crowded because once you get proteins folded you have tremendous efficiencies by having them so close together. You can pass very reliably an electron from one protein to another. But it does create this, and this has created throughout the history of living systems, has created this incredible problem in protein misfolding that gets worse and worse as we get older and older.
So having studied protein folding for a long time now, we got the idea that these devastating diseases-- and this is an example of a normal human brain in the brain of someone who's died of Alzheimer's-- that we might be able to study these devastating diseases in a simpler cell. So we're actually using yeast cells as sort of a living test tube to study this protein folding problem, and specifically to study what goes wrong when those particular types of proteins misfold, and those particular neurons. And so this idea-- this is a yeast cell, by the way, it divides by budding-- and they are very simple little cells. But they're not like bacterial cells.
So our idea was, they are not like bacterial cells, they are complicated cells, and I'll show you a picture again in a moment. But this was the way in which, when we first proposed to use yeast cells to study this problem of these neurodegenerative diseases, this was the general attitude that we were greeted with. And I have to say, it's an attitude that is very familiar to me, it's very much like the attitude that I faced when I decided I was going to get a PhD in biology lo many years ago. And that was talked about this morning.
It still continues in different ways. And one of the things that I've loved about MIT is that you can make some rather crazy ideas and propose them to your colleagues, and they don't actually laugh at you. They think, well, gee, maybe that would be interesting. So I want to thank MIT for being a wonderful environment in which we were able to do of this crazy sort of thing.
So the reason why we decided we were going to do this is that yeast cells, unlike bacterial cells, are really complicated cells. They're single cells, but they have all kinds of complicated machinery that characterizes all of our cells, including our neurons. And they have a very complicated cell cycle. They decide when to grow, and when to divide, and when not to divide in a very complicated way that's a lot like our cells.
They have all kinds of membrane-bounded compartments which traffic various proteins around in the cell. They have lipids and membranes. And they have complex systems for generating energy that are called mitochondria within them. And again, our nerve cells depend upon all of these things very, very intensely.
And this is just to remind you of that picture of a eukaryotic cell. And some of this is going to be featuring in my talk, so I just want to let you know what these green things are here. These green things are membranes. And they divide the cell up into several different compartments. And these membranes will bud off these little vesicles, and traffic those packets of other proteins to a different part of the cell. And neurons are particularly susceptible to problems with that going wrong, because they are huge, gigantic cells that have to traffic things from one end to the other.
So another aspect of yeast that made us decide to do that, is that there is no organism on the planet that we can manipulate as well as we can manipulate yeast. We know more about it. It has a very simple genome. The DNA was the first eukaryotic genome to be decoded. And it has certain kinds of properties-- that were actually first discovered by brewers trying to make better beer many years ago-- that allow it to be genetically manipulated in ways that are just like a dream come true for biology.
So we've got a really unrivaled toolkit for taking advantage of this organism. And because it's cheap to grow, and it grows very, very fast, we can do experiments in this organism on a time frame that is just staggering in comparison to the time frame it takes to do experiments in, for example, a mouse.
So I'm going to tell you, first of all, about some work that we've been doing with the synucleinopathies. And these are diseases like Parkinson's, dementia with Lewy bodies, and multiple systems atrophy, in which you see a particular protein, this alpha synuclein protein, misfolded in these different cell types.
And Parkinson's disease and parkinsonism, it's really part of a spectrum of disorders, and it's really the second most common of the neurodegenerative diseases. It's characterized by the loss of particular neurons dopaminergic neurons, and in particular regions of the brain, and of course the severe motor defects. It's a devastating illness. And there's a lot of bewildering things about this disease. There are some diseases that we know are caused by one particular change in one particular protein. But with this disease, there's a bewildering variety of environmental associations with toxins like manganese and mitochondrial poisons.
There's also clearly a large number of genetic factors that play into these diseases. And these, the loci that have been identified as being mutated in various people with parkinsonism, are called the PARK loci. And in the autopsy of those people, quite often you see in fact blobs of this alpha synuclein protein even when it isn't mutated. But interestingly, the very first parkinsonism gene to be discovered was in fact alpha synuclein. Because the mutation in that protein, or a simple amplification of the gene that is just making a few extra copies of that gene, is sufficient to cause parkinsonism. And it's a very simple little tiny protein that binds lipids and misfolds when it's not bound to lipids. And so we figured it might be a simple place to start in terms of trying to understand the biology of that protein, how it interfaces with different cellular compartments, and what happens when it misfolds.
So we took the alpha synuclein gene, and we put it on the regulation of a control element that we could switch on and off. And we fused the sequence of it to something called green fluorescent protein, which is actually a protein that biologists very broadly have borrowed from jellyfish. And it glows green when you shine blue light on it. So if it's used to tag the sequence of another protein, it allows you to follow that protein around the cell and actually look at it under the microscope.
So when we did that, when we put in two copies of the alpha synuclein gene into yeast cells, the protein did what we hoped it would do. It went to the membrane, the outer membrane of the cell. And that's great because in neurons this protein is found at the ends of the neuron, at the very farthest outer reaches of the nerve cell. And it's associated with membranes. When we put in one extra copy, things started to go wrong. When we put in two extra copies, like the amplification of the human genes in humans, things really went wrong. And in fact, these cells grow normally, these cells grow slowly, and those cells die. So what's great about that, is that gave us the opportunity to do genetic screens to try to find things that would make these cells grow better, rescue them. And we've done that with both this strain and this strain.
I'm going to tell you first about the genetic screen that we did with this strain here. We used the strain that was growing slowly, because what we wanted to do was be able to find genes that made the cells better or worse. And what we can do in yeast is what's called an unbiased genome-wide screen. That is, we have libraries of every single gene encoding every single protein in the yeast genome. And those are little plasmids. And we can put those plasmids, by genetic transformation, into a yeast cell that's also expressing this human protein.
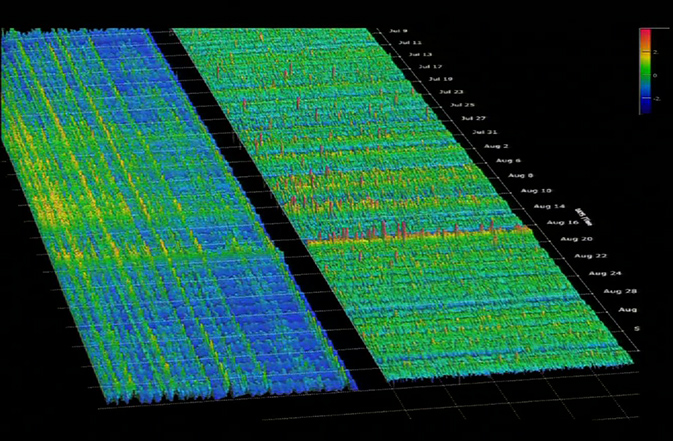
And as I said, the cells are growing slowly. And then we can keep those genes off until we want to start the experiment. And then when we want to start the experiment, we move them from the media where the gene is off to the media where both of them are now on. And we look for things that make cells better or worse. And the way the data looks is sort of like this. So what we have here is, cells that are not expressing that disastrous human protein, and they're growing just fine. When they are induced, they start to-- they slow down. They don't grow as well.
And we have every single gene that we've transformed. And we test in four independent strains so that we don't get things messed up by just sheer error. And so you can see here that these four strains all have one gene in it, and that gene is making the cells better. These four strains all have a different gene in it, that gene is making the cells worse.
Now the identities of those genes were really quite exciting. Because they looked like they might be involved in some of the biology that's been involved in parkinsonism. But that the yeast screen meant absolutely nothing until we actually took those genes, took the homologs, the related genes from other organisms, and tested them actually in a neuronal cell. So in fact, we not only tested them in a neuronal cell, we tested them in dopaminergic neurons, the particular cell type that suffers in parkinsonism.
And I'm just going to show you the results from-- Oh, there we go-- I'm just going to show you the results from our work with rat embryonic midbrain cultures. But I'll tell you that it worked in the nematode, and in the fruit fly, and there's various reasons why these organisms each have their own advantages and disadvantages for doing research. But since this is closer to home-- rats are, believe it or not, really quite similar to you-- I'll just show you the results here.
And I just want to mention that we are now taking this, we hope, to an entirely new level. Because this disease is such a complicated disease, we really believe this is really a kind of a poster child for the kind of disease that you would want to do personalized medicine with. And so we're collaborating with Rudolf Jaenisch's laboratory to make induced pluripotent stem cells from human patients with this disease. The goal being to try to determine how we can help the individual person based upon their underlying risk factors.
So in the midbrain cultures of the embryonic midbrain of rats, we culture those in a dish for a few weeks, and what we get out is about 7% dopaminergic neurons. And when we express alpha synuclein in those cultures using a virus, a lot of the neurons die, but the dopaminergic neurons die first. So there there's a difference and the percentage goes down.
And if we coexpress a random gene with that alpha synuclein, it doesn't help at all. But if we coexpress the gene that was our first strong hit in yeast, it rescues. And moreover, you can see from these little blobby things over here, there's been a defect in fact in the vesicle trafficking in those neurons. Those little globs of membrane that move around the cell and deliver neurotransmitters at the end of a neuron, those, there's a problem their trafficking. And our Rab1 one gene here turns out to be something of a protein that's involved in regulating that trafficking. And when you overexpress it in the presence of alpha synuclein, it corrects the defect that alpha synuclein causes.
So we've now done this with several other genes that were completely diverse in function. You would not have really guessed that they would be related to the vesicle trafficking defects. But these very, very diverse genes, every one that we've tested except for one-- and that's a pretty good ratio, we've tested several of them-- all of the human homologs of those genes actually fix the rat embryonic neurons. Or the nematode homologs fix the nematode brains.
So what we did then was with some biochemistry, and we were able to show that in fact what happens is that if you have vesicles, and you're looking for the budding from one compartment to the other, you can do that with some pretty fairly easy little assays. And you look for the changes in modification that take place in different compartments. And we found that in fact, when we did that with alpha synuclein, what happened was we had a defect in protein trafficking and the vesicles wouldn't fuse, and that's really bad news in a neuron. So let me just tell you about one of the other genes that we-- and that's why that Rab1 actually rescues that effect because it helps to move those vesicles forward.
So let me tell you about another gene that we hit, which at the time we first hit it had a very uninformative name. Its name is Yeast Open Reading frame 291W, because no one had any idea what it did. But it was of great interest to us, because when we looked in the human genome we found a homolog in the human genome that was a very high homology. And then up popped the following story. That people who have mutations in that gene will get early onset parkinsonism.
So our gene, when overexpressed, is rescuing the cells from the problem of alpha synuclein. That ties directly alpha synuclein function now to this other protein function. And we were able to use our yeast cells then to figure out what the function was. Which I think would have taken a very long time in mammalian neurons. And what we basically found was that this gene functions in manganese transport. In fact it functions and detoxifying manganese, which as I mentioned to you earlier is an environmental toxin, exposure which has been associated with parkinsonism.
Another thing we found was that mitochondrial damage, and this is just a genetic signature of the changes that are taking place in the gene expression profile of the cells that tell us that mitochondria, those energy generating factories in the cell, are getting sick. Remember I told you that there is a mitochondrial poison that is associated with environmental exposure to production of things like parkinsonism.
And so, again this nucleon is tying all these things that have been seen in human neurons together in our yeast cells. So that allowed us to do a chemical screen for compounds that would rescue the yeast cell. And we screened 150,000 compounds. And we were able to do this in a very short period of time relative to screening in neurons. We asked for something simple like restoration of growth in that extremely high toxicity strain. Because in that high toxicity strain, that's where all those different things are going wrong. The problem with manganese, the problem with mitochondria, the problems with proteins moving around the cell.
So we want to see if it might be possible to find a compound that would rescue. And we only got a few. It's an extremely rigorous screen. But in fact when we looked at the cells, they fixed the problem in trafficking. They fixed the mitochondrial defect. And they worked in nematode and rat neurons too. And moreover, they not only provide protection in rat neurons from alpha synuclein toxicity. They provide rescue from a mitochondrial poison to which I mentioned that environmental exposure can cause early onset parkinsonism.
And so here's just a simple little snapshot of that. This compound is called rotenone. And these are neurons in a dish that are mostly dying because of the rotenone. And if in the presence of one of our rescuing compounds, these neurons obviously look an awful lot better.
So what we can tell, then, is that this particular protein is causing very specific neuropathology. Particular types of neurons are dying. But the reason it's doing that is not because it's affecting a process that's specific to neurons. It's that it affects a very general basic cellular process that all cells need, but that dopaminergic neurons are simply particularly sensitive to. And so those cells die first. The individual dies. And you don't notice that in fact, there's lots of problems everywhere else.
So why dopaminergic neurons? We think it's partly because neurons are so highly dependent on trafficking. Because they're so long and they have to move things at such long distances. And they communicate with each other with these little vesicles releasing packages of signaling molecules to other neurons.
And we think that the high local concentration of those kind of bowling balls of alpha synuclein aggregation that I showed you is responsible for another feature that that's toxic, which is that the aggregates themselves can be toxic. There's a special vulnerability to metals which we're still unraveling. But it's clearly true for both the neurons and the yeast cells when this synuclein that's misfunctioning. Neurons have particularly high rates of respiration, hence they're particularly dependent upon their mitochondria.
And then finally dopamine is normally made out in the cytosol. And it's a dangerous neurotransmitter. It needs to be packaged into these vesicles right away, or it breaks down the cytoplasm and does bad things. And so if there's a defect in the production of these little membrane-bounded vesicles in the cell, it's going to affect a dopaminergic neuron more than most neurons.
So we're beginning to understand some of this special vulnerability. And beginning to think that there might be a more rapid route to trying to find some therapeutic targets for this disease.
So I want to finish by telling you something we haven't published yet. This is some work we're doing to look at the toxicity of Abeta, a peptide that accumulates in the brains of Alzheimer's victims, which is the number one cause of neurodegeneration in humans. And with all of us living longer, healthier lives, we are all facing the prospect of getting this disease.
Abeta is a little tiny peptide that's actually made in the brain in a rather complicated way. It's made from a much larger precursor protein and there's a couple of different enzymes that are involved in clipping it into this small little peptide here that's prone to misfolding. And so in humans that protein is trafficked, again, through these very complicated pathways.
It starts out in something called the endoplasmic reticulum. Then it moves to something called the Golgi. Then goes to the plasma membrane. It comes back into the cells and something called the endosomal compartments. And it's believed that it's processed into this Abeta peptide in all of those different places. And it's believed that this external stuff out here is perhaps some of the most dangerous stuff when it gets out there, alone and loose by itself, and can form [INAUDIBLE] species.
So how do we ever reproduce this in a yeast cell? Well, we skip that whole processing step to begin with. And what we do is we take a little signal sequence that will get the protein delivered into the endoplasmic reticulum. And we just take the Abeta sequence itself, nothing else. So when we put that gene into a yeast cell, when the protein starts to be made, the protein first gets delivered to the endoplasmic reticulum.
And then there's a cleavage system in that that's very, very highly conserved. And it cleaves that protein and makes just the simple little Abeta peptide. Which then is free to move into the other compartments of the cell with a series of vesicle fusions, which I don't have fully animated on this particular slide. It gets delivered to the outside of the cell.
And what's cool about yeast cells is that they've got a cell wall. So that means, when they make their Abeta it's not going to just to diffuse away. It's going to stick close to the plasma membrane, which is believed to be one of the most dangerous sites for susceptibility to Abeta. And it's going to come back in. And so we set up cells, and we did the screens in exactly the same way that I just showed you for alpha synuclein.
And we've, as I mentioned, we're just getting ready to submit this paper, but I wanted to just tell you about it because I'm really quite excited. We've hit a variety of different genetic modifiers of Abeta toxicity, many of which have homologs in humans. And we found that clathrin mediated endocytosis, three of the genes were all involved in that one pathway. And this gene here, which is involved in that in that endocytosis, that taking things that have hit the plasma membrane and bringing them back into the cell.
One of them is PCALM. And it turns out that in the human genome-wide arrays that have been used to try to find genetic risk factors in human beings for Alzheimer's disease, PCALM is the third highest hit. So it's a very, very well validated protein that's involved somehow in Alzheimer's disease. But there was really nothing to link it directly to Abeta. In fact, the hypothesis of how it was working was not through Abeta. So we think we've uncovered that.
We also have two additional connections to unpublished data that I'm not at liberty to talk about here. I just want to mention that we have set up now a nematode model for this disease process. And again using green fluorescent protein you can visualize the neurons of the nematode here. In particular we're looking at the glutaminergic neurons, which are the most relevant neurons in Alzheimer's disease. Nematodes, lowly as they are, they have these different types of neurons.
And when we express Abeta in those cells, we don't get as many of the neurons. And this is a very dramatic change, believe it or not. Because nematodes, one of the reasons they are such a darling for research, is that every worm always develops with exactly the right number of neurons. But here Abeta is causing some of those neurons to die. And you can see that here is, it's an age-related neuronal death. 40% of the worms are normal at three days, and fewer are normal at seven days. So there's age related neurodegeneration going on.
And if we express two other random genes in those nematodes, it has no effect whatsoever. But if we take our modifiers from the yeast screen, the things involved in clathrin mediated endocytosis rescue. Three other genes with completely different functions rescue. And one of the genes that makes the yeast cells worse makes the nematode neurons worse as well.
So, data just in. We've also done this now with rat primary cortical neuronal cultures. And they are also affected by the Abeta. And they're also protected from Abeta by PCALM.
And finally, what gives us quite a bit of hope is that there's this compound, it's the only compound that's been shown so far to rescue a mouse model of Alzheimer's disease that actually reduces the burden of Abeta and restores cognition and learning and memory. These are yeast cells growing without Abeta. These are yeast cells not growing with Abeta. And this is the rescue of our yeast cells with that chemical compound.
So we have just been given a grant to screen 350,000 compounds at the MIH for compounds that might rescue yeast cells and cross over into neurons. So that's all I have to tell you, except I hope this is the tip of the iceberg. I'm not sure it will be or not. We have a long, long, long way to go. But I want to thank the extraordinary young people in my laboratory who did this work. These are the people who set up the synuclein. These are the people who did the second stage. And these are the people who did the Abeta work, which is as I mentioned not yet been published. And these are our wonderful, wonderful collaborators. Science has become much more collaborative over the years. And in order to make progress we are making, we really use the help of these people.
So that's it. Thank you. And I'm happy to answer questions, or did you want to take questions after, or would do you want to do?
SIVE: Questions... Questions now.
LINDQUIST: Yes.
AUDIENCE: What's the mechanism for the neurotoxicity of [INAUDIBLE] Abeta?
LINDQUIST: Well it's been not well understood. It's quite clear that there's something about the misfolding of that protein. And it's thought to be that the misfolding of that peptide creates a variety of surfaces that have a hydrophobic character to them that interact with membranes and punch holes in membranes. But it hasn't really been entirely clear.
And that's why being able to do genetic screens, genome-wide, without any preassumptions of what this protein is doing, the genetics, the things that we get that correct the defect, tell us about what is going wrong. And so the fact that one of the genes that we're getting is a gene that's involved in grabbing things from the membrane and bringing it inside the cell, and dumping it into a vacuole or compartment for degradation, tells us that that membrane and that trafficking process is part of the actual reason for the toxicity of Abeta protein. Yes.
AUDIENCE: If you're screening compounds, how do you select the compounds to screen?
LINDQUIST: Yeah, so the first library that we've screened was a library of compounds at the Harvard Institute of Chemical Biology. And they've actually gathered compounds from all over the world. All sorts of different places, from failed pharmaceutical companies, and from when the Soviet Union shut down they grabbed a bunch of the compounds their chemists were making, et cetera. Now, more recently what we're going to be doing with NIH, is the National Institutes of Health has put together a library of 350,000 compounds that are new compounds, that are easier to resynthesize, that are cleaner.
And they are setting up screening centers at several different places. We're doing some screens at the Broad. Also doing some screens at NIH itself. And they actually have all kinds of very fancy robots that allow academics to come into those facilities and do things that normally an academic lab could never have done before. So it's a very large collaborative effort.
AUDIENCE: What's rotenone?
LINDQUIST: Rotenone is a toxin that hits a particular enzyme in the mitochondria and causes the breakdown of that energy-generating system.
AUDIENCE: [INAUDIBLE]
LINDQUIST: I don't know, but-- I don't know where it's actually synthesized from. But it's a pretty terrible compound. It's a compound that's used actually, for example, for killing fish in ponds by certain individuals who want to harvest fish rather quickly, rather than using a line and pole. And it's used in many other places in the environment. There are a lot of people who are now really quite alarmed by the fact that it is being used out in the environment.
Any other questions? Thank you all very much.
SIVE: Thank you so much, Sue, for sharing your really groundbreaking research with us. I'm going to take my glasses off so I can read what I have in front of me here.
The theme that we organized this session around spans departments, and spans schools, which is really one of the things about MIT-- research spans so many departments and schools, and life sciences research particularly spans the schools and the departments very broadly at MIT. And we continue with a life sciences theme, and with the theme of faculty who are addressing huge issues in human health with our next speaker, Professor JoAnne Stubbe.
Professor Stubbe is the Novartis Professor of Chemistry and Biology at MIT. She received her BS from the University of Pennsylvania and a PhD in organic chemistry from the University of California at Berkeley. After taking faculty positions at Williams College, Yale, and the University of Wisconsin, she happily joined the MIT faculty in 1987.
Professor Stubbe analyzes the mechanisms of ribonucleotide reductases, enzymes that are pivotal in DNA metabolism. She studies natural product DNA cleaving agents that impact development of new cancer treatments and environmentally friendly polymers.
She's been broadly decorated. She was elected to the National Academy of Sciences in 1992, was the recipient of the American Chemical Society's Nakanishi Prize, the Benjamin Franklin Medal in Chemistry, and in 2009 received our nation's highest honor, the National Medal of Science.
The title of her talk today is: "Radicals: Your Life in Their Hands!" Professor Stubbe.
STUBBE: Okay. Boy, I'm really nervous. Anyhow, I would like to begin by thanking the organizing committee for inviting me to participate in this symposium celebrating the contributions of women in the School of Engineering and the School of Science. I'm really flattered to be here. Second, I would also like to thank MIT for providing me over the last 20-- almost 25 years, with such a stimulating and intense environment to carry out my passion. And to providing-- to allow me to have access to outstanding graduate students who are motivated and enthusiastic. And also finally to have access to colleagues across all disciplines, some of whom are shown here, that have allowed me to push my science forward in ways that I never could have imagined.
Okay, so today I'm going to be talking about radicals. Your life is in their hands. And I hope by the end of my talk you have some idea what that title means. Okay, so what is a radical? Radicals, if you look it up in the dictionary, have many definitions. To a chemist, biochemist, or biologist, a radical is a molecule with an unpaired electron in its outermost shell that's chemically extremely reactive, and it's dying to pick up a second electron and form a covalent bond.
And so radicals, being highly reactive, are also considered to be highly destructive. And so most radicals, when people think about it in biology, are bad radicals. And in fact, if you look in the literature, each month there are literally hundreds of papers published on reactive oxygen species. And reactive oxygen species are reductive metabolites of oxygen gas, an unavoidable consequence of the fact that we live in an aerobic world. Radical species can also be generated by light. These reactive radical species react indiscriminately with whatever they encounter. So they react with small molecules. They react with proteins.
And here is a cartoon of our genetic material, that Susan just talked about, DNA. And when they get encountered DNA, they form a covalent modification, a stable modification, leading to a mutation. And if the mutation is not repaired and you replicate your DNA, these mutations ultimately contribute over a period of time to the aging process and to disease states. So in fact, organisms have evolved many ways to try to remove or annihilate these free radicals. So, for example, my sister goes to the health foods store at least once a month to buy vitamin C and vitamin E. These are antioxidants that can trap these free radicals, preventing them from doing damage to our DNA.
If, in fact, our small molecules that have been evolved to inhibit these free radicals escape then nature has also evolved many proteins or enzymes that can figure out that the DNA is damaged, and then can cut out the damage, and repair the damage. And those enzymes, DNA repairing enzymes then prolong our advances towards the aging process and disease. So in general, when people think about radicals in biology, they think about destruction.
And so today what I want to do is talk about good radicals in biology, and that's my take-home message. That, in fact, nature has figured out how to harness the reactivity of these radicals to do extremely challenging chemistry with exquisite specificity. And so in the next few slides I just want to show you-- I was hoping some of my 507 students would be in the audience, but I haven't seen many students-- that many of the things they learn about in introductory biochemistry that involve more conventional two-electron chemistry also involve radicals.
So for example, many of the metabolic steps that occur inside all cells require cofactors. And these cofactors are derived from vitamins. And so here, vitamin B1 is involved in the pentose phosphate pathway, vitamin B2 is involved in redox chemistry, vitamin B6 is involved in amino acid metabolism. Well, conventionally everybody thinks these cofactors do chemistry two electrons at a time. In fact, they catalyze chemistry as well by one electron, or radical chemistry.
In addition, vitamin B12 is converted into nature's most beautiful cofactor. It's bright pink, adenosylcobalamin. And it has been a paradigm for thinking about radical mediating chemistry to generate this reactive species involved in fatty acid metabolism. I think the most amazing observation that has been made about radicals is that in the last decade it is now known that S-adenosylmethionine-- and so this is, you learn in introductory courses, a universal methylating agent. It methylates small molecules, it methylates proteins, it methylates RNA, it methylates DNA.
We now know from biochemical studies, and also from genomic analysis that SAM can mediate over 3,000 reactions that involve free radical chemistry. And the reactive intermediates are exactly the same as the intermediate that's generated by B12. So I think it's widely underappreciated how important radicals are in normal metabolic pathways.
But even more underappreciated, I think, is the fact that nature uses our proteins a specific amino acid with these proteins, and converts them to radicals which do really important chemistry. So in fact, many people at MIT now, we're in the post-genomic or proteomic era, have studied post-translational modification of proteins that changes their regulatory properties by phosphorylation, methylation, acetylation. Most people do not realize that we have post-translational modification by oxidation. And in fact this oxidation involves metal base cofactors. So here are the normal amino acids: tyrosine, glycine, tryptophan, and cysteine. And all of these radical species are now known to play a role in a number of reactions involved in primary metabolism.
And today I'm going to focus mostly on a tyrosyl radical. Tyrosyl radicals in solution have lifetimes on the order of 10 to the minus 3 to 10 to the minus 6 seconds. Yet in the enzyme that I'm going to be talking to you about today, it can have lifetimes, depending on the organism, from 30 minutes to four days. And tyrosyl radicals play a central role, as you'll see today, in making the building blocks, the deoxynucleotides required for DNA biosynthesis.
But it goes beyond that particular step. In fact, we now know that a major mechanism of oxidation of water to oxygen gas, everybody is interested in that because of the energy problem, involves a manganese calcium machine and transient tyrosyl radicals. And so plants, and Prochlorococcus-- you'll hear a lot about that from Penny Chisholm later on, I think her talk is tomorrow-- can convert water into oxygen using light for the energy of this uphill process, and using transient radicals, tyrosyl radicals. Transient tyrosyl radicals are also involved in the target of aspirin and non-steroidal anti-inflammatories like ibuprofen or Tylenol. And so tyrosyl radicals play much more, and I think underappreciated, roles then people-- normal biochemists actually think about.
So today what I'm going to be doing is talking about tyrosyl radicals and sulfur radicals in the role of the system that we've focused on for over 30 years. So my laboratory has spent a lot of time studying ribonucleotide reductases, RNRs. The genes that code for these enzymes are called nucleotide reductase genes, or the "nerd" genes. And so I'm often reminded that it's appropriate that I'm at MIT.
Anyhow, ribonucleotide reductases in all organisms, from bacteria that grow on methane gas to humans, catalyze the conversion of nucleoside diphosphates, all four of them here, into deoxynucleoside diphosphates. Providing the appropriate ratio required for DNA replication and repair and the appropriate amounts, both of these are essential for the fidelity of DNA replication and repair.
And so today what I want to do is tell you how radicals are involved in this nucleotide reduction process. I also want to mention that the central role in nucleic acid metabolism in general has made these enzymes a successful target now of three drugs that are used clinically.
So this is the actual reaction that the enzymes-- that the ribonucleotide reductases catalyze. This is a nucleotide. This is a precursor to RNA. This is a deoxynucleotide. This is a precursor to DNA. Ribonucleotide reductases catalyze cleavage of a carbon hydroxyl bond and formation of a carbon hydrogen bond. That's a reduction process, and the reducing equivalents are provided by two cysteines that get oxidized to a disulfide.
Now in addition to these two cysteines, we showed in the mid-90s that there was also a thiyl radical involved in this transformation. I think it was unanticipated that a reaction that looks pretty simple would involve complex free radical chemistry. So what happens is this thiyl radical initiates this process by cleaving this bond, removing a hydrogen atom. And I will spare you the details of the mechanism, but we spent many years trying to understand how this process works.
So this raises a question. Where does this thiyl radical, or cysteine radical, come from? And so we now know, we've gone through the age of genomics, proteomics. We have had a revolution in structural biology. We now know by putting all-- and biochemistry-- putting all this information together, that there are three classes of ribonucleotide reductases. They all share an identical active site, shown here, where the nucleotide is reduced to a deoxynucleotide. So here's the substrate, the nucleotide. Here are the two cysteines that provide the reducing equivalents. And in a finger loop through the center of this ten-stranded barrel, you have a cysteine that needs to be oxidized to a thiyl radical to initiate this process.
So then you ask, how do we define these different classes? And the classification is based on this cloud. And this cloud, which I will unveil in a minute, provides an understanding of the mechanism by which this oxidation occurs. So we'll see that nature has probably by divergent evolution made a common machine to convert nucleotides to deoxynucleotides, but the mechanism of oxidation differs.
So in the class II enzymes-- here is nature's most beautiful cofactor again-- she uses B12. Here is the cloud unveiled. That's the structure part of the B12 molecule. Ribonucleotide reductases in the class II are found in both prokaryotic systems and a few eukaryotic systems.
The class III enzyme shows you another molecule I showed you at the very beginning. SAM, S-adenosylmethionine, which generates the same reactive species and generates a protein radical, a glycyl radical. And this glycyl radical then mediates the oxidation. And so here is the glycyl radical sitting right next to the cysteine that needs to be oxidized.
Here is adenosylcobalamin sitting right next to the cysteine that needs to be oxidized. And this chemistry happens over a few angstroms by direct hydrogen atom obstruction. The class III enzymes are found only in organisms that can grow under strictly anaerobic conditions.
But the one most of us who have spent our time on is the one that's found in humans. And this is the class I ribonucleotide reductases. And what you see if you look over here, here is where the cloud was, that in place of the cloud now we see two tyrosines. But tyrosines are unable to carry out an oxidation of a cysteine to a thiyl radical.
So the question is, how can that happen? And the answer is that when you purify this protein-- again, this is common to all ribonucleotide reductases-- you find in the class I enzymes a second subunit. And this second subunit is different in different organisms, although it's structurally identical.
And so we've subdivided the I class into A, B, and C based on the unusual metallocofactor. So the metallocofactor in human organisms has a diiron center. And the function of this iron center, which needs to be made biosynthetically, is to oxidize tyrosine to a tyrosyl radical.
This is the oxidant, remember in solution, and it has a very short lifetime. In the active site of the human enzyme it has a lifetime of 30 minutes. So something is unique about this system. If you reduce this tyrosyl radical back down to the amino acid tyrosine, your enzyme is dead.
Only in this past year, my lab and a laboratory from Germany discovered another ribonucleotide reductase. This one has a dimanganese tyrosyl radical cofactor. And this cofactor appears to be unique to pathogenic organisms.
Finally, the class I C ribonucleotide reductases was discovered by one of my former students in 2005. This structure is found in human intracellular parasite chlamydia. And it has an unprecedented metal cluster, manganese 4 and an iron 3.
So now the question is, how do these tyrosyl radicals in this manganese cluster oxidize a cysteine, which it turns out you will see in a minute these guys are 35 angstroms removed from the cysteine that needs to be oxidized. So the model is the following. This is the common structure of all ribonucleotide reductases. This is the place where nucleotides are reduced to dioxane nucleotides. This is the center where we need to oxidize a cysteine to a thiyl radical.
The second subunit is the one I just showed you on the previous slide. Here these two balls are the iron clusters, and the iron center is involved in the oxidation post-translational modification of tyrosine to a tyrosyl radical. From this model, this is tyrosyl radical is located 35 angstroms away from the cysteine that needs to be oxidized.
So no matter what you do you, you learn from basic biochemistry that electrons and oxidation in reduction centers are usually spaced on the order of 10 to 15 angstroms. If you go much farther, the rate constant [INAUDIBLE] can become so slow that you can't do chemistry. So the question is, how does this oxidation occur?
And so this is the working hypothesis in the field, which I think we've obtained quite a bit of support for in the past few years. So here is the subunit with the iron cluster that generates this tyrosyl radical. And in E.coli, this radical has a lifetime of four days. Over here is the subunit that's common to all ribonucleotide reductases where the nucleoside diphosphates bind, and deoxynucleotides are going to be made.
Here is the cysteine that needs to be oxidized. But we see no metals between the tyrosyl radical and the cysteine. So we're forced to use aromatic amino acids, which are easy to oxidize to catalyze this oxidation in a process that we believe involves proton-coupled electron transfer.
And electron transfer, they're very small so they can tunnel over very long distances, 10 to 15 angstroms. Protons are 2,000 times bigger. They can only tunnel under over about 7/10 of an angstrom. And so we need to evoke loss of a proton, as well as an electron at each step.
This is a major focus of many laboratories now understanding this kind of a process is it's intimately linked to the photosynthetic reaction process and to the energy problem. So the model is the following. This guy is going to reduce this guy and you're going to pick up a proton generator radical. Transfer a proton.
This guy is going to reduce this guy, and you're going to pick up a proton. This guy is going to reduce this guy. This guy is going to reduce this guy. This guy reduces that guy.
You generate the sulfur radical. Now, you do all the chemistry over here. Nucleotide is converted to deoxynucleotide. And believe it or not, you have to go back. And this happens on every turnover.
Now how silly is this? It seems like the enzyme could kill itself very easily by carrying out this kind of a process. On the other hand, I think studies that we've done in the last few years where we've used new technology we've been able to cite specifically incorporate unnatural acids into these proteins where we can perturb the reduction potential, which is involved in the oxidation process and the ability to lose a proton, which is involved in the proton process. We have very strong evidence for that pathway I showed you on the previous slide. And we're now in the process of studying the details of proton-coupled electron transfer.
So what have I showed you? This is the class I enzyme. Here's where the chemistry happens. Here is where the tyrosyl radical is found.
This was the first protein in 1978 that was discovered to have a tyrosyl radical. My laboratory of many years has unraveled the chemistry by which the oxidation occurs and by which this cofactor is assembled inside the cell. It's now clear that metals certainly don't float around inside the cell. They use complex biosynthetic pathways.
The chemistry of nucleotide reduction and the importance of a cysteine radical all occurs on this subunit, and we spent a lot of time studying that. And this oxidation occurs over a long range, over 35 angstroms by a very bizarre mechanism involving proton-coupled electron transfer. OK. So I've shown you that ribonucleotide reductase is a veritable playground for free radical chemistry. It's also important in terms of translational chemistry.
So we now know that RNRs is a successful target of a number of drugs that are used clinically, one of these clofarabine from Genzyme. Part of its cytotoxicity is related to an inhibition of ribonucleotide reductase. It's used in treatment of refractive lymphoblastic leukaemia.
Gemcitabine is a Lilly drug, but it was designed by a group at Miriam [INAUDIBLE] based on all of the chemistry we unraveled. It's a stochiometric mechanism-based inhibitor of ribonucleotide reductase. Hydroxyurea, which many of you might have used in the laboratory, but it's also used in combination chemotherapy treatment of hematological cancers, while everybody believes it destroys the tyrosyl radical, in reality we believe it interferes with this hopping process between the two subunits.
[INAUDIBLE] is in phase II clinical trials. We don't really know much about its mechanism, but it destroys the iron center and the radical and activating the enzyme. And in all class I ribonucleotide reductases, the interaction between the two subunits is quite weak governed by a C-terminal tail, which is distinct between humans, viral, and bacterial enzyme. Again, disruption of this interface is therefore another option for inhibiting ribonucleotide reductase.
So in the last few slides, I'm going to go back to the theme of good radicals, bad radicals. So here is the ribonucleotide reduction process. Nucleotide to deoxynucleotides. Two cysteines get oxidized to a disulfide. And here's our sulfur radical generated by a tyrosyl radical.
While I won't go through the details of the chemistry, the first step in all ribonucleotide reduction reactions is removal of a hydrogen atom, generating a nucleotide radical. And then you do a lot of dots. That's a radical. You do a lot of these dots before you get to product.
So these are good radicals. We've calculated you can do 5 million turnovers, and the enzyme never kills itself. So nature has figured out how to harness this reactivity to do this really tough chemistry.
On the other hand, when you make a simple conservative substitution, you replace a hydrogen and a hydroxyl with two fluorines, or a hydrogen and an azide, basically, all hell breaks loose. And both of these compounds are stochiometric mechanism-based inhibitors of ribonucleotide reductase.
So mechanism based simply implies that these reactions are chemically very stable until the sulfur radical removes a hydrogen atom. That's what happens in the normal reaction starting this process. And then the chemistry goes nuts.
During this reaction, you lose two fluorides, an azide, which goes off as nitrogen gas. You cleave the base from the sugar. You lose pyrophosphate. And you're left after you cleave all these bonds with this sugar species, which irreversibly and covalently modifies the enzyme, killing it.
So what have I told you about ribonucleotide reductases? They are a playground for radicals. It's the first example of a thiyl radical that was demonstrated in biology. The thiyl radical is generated by a tyrosyl radical, which involves unprecedented iron chemistry, which we now know is prevalent in many systems.
The oxidation process over a long distance of the tyrosyl radical to a sulfur radical involves bizarre hopping mechanism through aromatic amino acids and is serving as a paradigm for proton-coupled electron transfer. RNRs are the successful target of drugs that are used clinically. And the last little bullet for those of you who like to think about evolution-- I guess I'm getting old enough to start thinking about evolution-- if you believe in an RNA world and the ribosome makes polypeptides, how do you get to a DNA world? You must use ribonucleotide reductases.
So finally, I'd like to thank these are the members of my current lab group. They work on things that are really hard and really challenging. And they remain enthusiastic despite all the problems. And as I said earlier on, none of my science would have been possible without the spectacular collaborative efforts I've had with people within MIT and all over the world. And thank you for your attention.
[APPLAUSE]
MODERATOR: It would be nice to be slightly less casual about questions. And so if you do have a question, please do come up to the microphone. You can pick it up and take it back to your seat. That would be quite fine.
STUBBE: All right. No 507 students out there asking me why I don't teach about radicals in my introductory course? No. OK. All right.
AUDIENCE: [INAUDIBLE] question from someone [INAUDIBLE]. So this spectacular oxidation process that you showed. Does that work in a cell or does that work in solution or do you think it needs to be crowded so it works?
STUBBE: So these are all in the active site of the enzymes. The ribonucleotide reductases are enzymes so they're sitting in a protein environment. And so you have two proteins that come together. And you would think that if the electrons started hopping it would be all over it. They would get quenched and that the enzyme would be dead since you would be destroying your tyrosyl radical.
But in reality, the whole process is conformationally gated. So it's only when you bind the substrate, the nucleoside diphosphate, they have dioxynucleotide effectors. When you bind those then the conformational change is triggered. And you do this electron transfer process.
So everything is ready to go. The reactions are all extremely fast. So the only way you can see intermediates like what I showed you and what we've identified is actually by perturbing the system. So usually an enzyme reaction to chemistry over eons of years has evolved to be perfected. And the rate limiting steps are all physical steps or conformational changes.
So to see the chemistry you have to perturb the system, which is what you do studying enzyme mechanisms. I don't know if that answered your question or not. But you should take 507. It's a great course.
MODERATOR: Thank you so much, Joanne, for really a fantastic talk.
[APPLAUSE]
MODERATOR: The thing is we didn't want to just feature our scientists and engineers whose star had risen and was shining brightly in the sky to speak. We also wanted to feature our slightly more junior faculty whose star had risen and was, perhaps, still rising. The analogy gets a little forced, but you understand where I'm going here.
And so I would like to move on to our next speaker whose focus is also a life sciences biomedical focus, but who is at it's slightly earliest stage of her career than the speakers that we have already heard this afternoon.
Professor Sangeeta Bhatia is professor of health sciences and technology and professor of electrical engineering and computer science at MIT. She received her BS from Brown, her MS in mechanical engineering from MIT, and then in the joint MIT Harvard HST program, her MD and PhD in medical engineering and medical physics in 1997 before subsequently joining the MIT faculty.
Dr. Bhatia's research is focused on the applications of micro and nanotechnology to tissue repair and regeneration with emphasis on biology of the liver. She is the recipient of a Lucile and David Packard fellowship and an NSF career award. In 2003, she was elected a fellow of the American Institute for Medical and Biological Engineering. And in the same year, named one of MIT technology reviews 100 top investigators.
The title of her talk is It's a Small World, Tiny Technologies in Medicine. Professor Bhatia.
[APPLAUSE]
BHATIA: Good afternoon. So as was mentioned, I'm going to tell you about the role of tiny technologies in medicine. I want to say it's a real pleasure to be here. I'm so proud of MIT for having this symposium and for the progress we've made in highlighting gender equity issues in science and engineering.
OK. So I'm going to tell you today appropriately about our interest in communities. And in particular, I'm interested in the idea that communities are collectives of individuals that have some identity or behavior. And these communities function because of the interdependencies amongst the individuals in the community. So a single individual responding to its local environment can negatively perturb a community or positively perturb a community.
And in particular what we're interested in is how these interdependencies work in living systems at smaller and smaller length scales. So if one thinks about this idea of community, in fact, there are a whole disciplines devoted to how communities function and how this interdependency works. So at the level of community, social community, we have sociology. If we think of an individual human being and we think about the interdependencies between the organ systems that's the study of physiology. And if we go down and down in length scale all the way to a single cell and we think about this different signaling pathways that are interacting, we now have a new discipline that people are calling systems biology.
So we've been interested in is the interdependencies of individual cells down here in the tissue microenvironment. So you're looking here this is a liver. This is a functional unit of the liver. And these are now hepatocytes liver cells inside the liver.
You can see in this tissue and in any tissue there are at least 5 or 6 different cell types, all coordinating the function of that issue. In fact, we're interested in studying the role of the microenvironment around these cells and the influence on the cells, and then how they orchestrate that tissue function for better, for health or for worse, for disease.
OK. So it turns out, what does this have to do with tiny technologies? Tiny technologies, one of which is I'm going to show you here, are wonderful tools for interrogating the cellular microenvironment, which is about 100 microns around living cells. So what I'm showing you here is the power of progress that's been made through miniaturization.
This is a single transistor to 100 million transistors over the course of 50 years of concerted effort, and this drove the computer revolution. This is why our computers get faster and faster every year. And this computer revolution was driven largely by a simple manufacturing process, and that's called photolithography. So photolithography is the coding of surfaces with light-sensitive polymers, shining light through a mask, and the ability to pattern those surfaces.
In using these patterns, you can pattern resistors and circuitry like you see here at very high density, smaller and smaller length scales. So we and many others have been thinking about how these kinds of techniques can be literally borrowed for applications in biology and medicine and in particular, as I told you, I'm interested in how they could be useful for understanding communities at the cellular length scale.
So there's been a lot of work in this field in general, and I just want to kind of orient you to this space. So there's something called top down manufacturing, which is the process that I just described to you. And what's been done in sort of the non-living medical applications, so in the bio analytical space, are things like this.
So here what you're looking at is a microfluidic chip, which has been molded off of a surface that was patterned like I showed you on the last slide. And these lab on a chip devices are useful now for point-of-care diagnostics, for measuring glucose from a single pin prick of blood, and so on. If you go down to smaller length scales, you can print things at the 100 micron length scale using some of these same technologies. This is the way that DNA microarrays are made. So this is how affymetrix chips are made using the same kind of process except for instead of, again, printing circuitry, you're printing molecules.
And so as the technology gets better and better, you can actually start to approach the nano scale from what we call the top down. Now conversely, what's going on, which is very exciting, is that there's so-called bottom up manufacturing processes emerging. So this is actually a fluorescent semiconductor nanocrystal that's about 3 to 5 nanometers in size when it's uncoated. And when it's coated it's about 50 nanometers in size.
And these materials have fascinating properties they have, for example, shape-dependent color. So you can shine blue light on all of these materials and they glow depending on the shape, the size that they are. So folks have been interested in accessing the same length scale that I mentioned earlier by taking these nanomaterials, which you can solution synthesize, and assembling them into larger and larger structures. And so we call this bottom up manufacturing.
And so what I hope to convince you of today is this forms a wonderful repertoire of tools for us to access the 500 to 50 nanometer length scale. This is the perfect length scale for studying the cellular microenvironment in tissues.
OK. So our interest is in the liver as I mentioned. And what I'll be telling you about in the next few minutes is how we're interested in building complicated microenvironments, building liver tissue where the liver cells are happy enough to perform all the functions about that I'll tell you in a second so they can be therapeutically useful.
We're interested in making arrays of miniature versions of this liver tissue so that we can study new pharmaceutical drugs that will one day be in people and try and make them safer. And we're also interested in studying the interaction of a healthy liver with an infection, with hepatitis C for example. OK.
So how do tiny technologies help us with this? So first, I just need to orient you to the liver, which you might not have thought about in a while. The liver has about 500 functions, which is surprising. It's about the size of a football. It sits in the right upper quadrant of your body.
And we bucket the 500 functions into these four main categories. Detoxification of drugs, protein synthesis, energy metabolism, and production of bile. Liver failure is sadly a lethal disease, and the only treatment option yet to this day is whole organ transplantation. So there's very limited number of organs available. And we and many others have been interested in coming up with alternatives for whole organ transplantation, that is an engineered liver that you would implant off the shelf if you will.
In this construct, this implantable construct, you would fabricate this in the laboratory from cells that do all these 500 functions and materials, culture them in vitro, and then implant them into patients. Now the challenge has been in realizing this vision that these 500 functions are rapidly lost in culture. So if you take these liver cells out of the microenvironment in the liver-- and this is an artist's rendition of the microenvironment of the liver-- you put them in a material system, this is what happens to their function.
So this is just one of their 500 functions, but they all do this, and that is that they rapidly decline and the cells go on to become what we call fibroblastic. So hepatocytes are an epithelial polarized cell, and they lose their function very rapidly. OK. So this has been known for quite some time. And you can't harness the function of these cells then if you can't preserve it.
So in the early '80s, a seminal piece of work was done by this woman researcher, Christiane [? Guguen Guillouzo. ?] She made the observation that if you added other cells from the liver back to these cells that had been isolated you could rescue their function, at least transiently. And we call that the co-culture effect.
When I was a graduate student here at MIT in the '90s, we got interested in studying that more and using it for some of these therapeutic applications. And in particular, we were interested in using these tiny technologies that I mentioned for organizing these co-cultures. So instead of making a co-culture like you see here where the liver cells, the hepatocytes are red and the supportive cells are green and everything is disorganized, instead we could use those same techniques that I described to you earlier where you shine a light through a mask on a light-sensitive polymer-- in this case, on a glass cover slip-- to coat it with sticky proteins-- in this case, collagen-- you could organize the cultures. So you could go from random co-cultures to what we call micropatterned co-cultures.
We had single cell precision on which cellular neighbors were present in our cultures. And what we found was depending on the architecture of the tissue we could tune the level of function, that level of rescue of liver-specific function, and the length of function. So we could extend the function of the cultures from a day to about two months for rodent cultures and about one month for human cultures. So we're not done yet, but that was progress.
The other thing we were interested in doing-- you could play the movie please. They told me to say that. You can roll the movie please. There we go.
We were interested in the dynamics of this cell-cell interaction. So we used another technique that emerged from the world of tiny technologies, and that's actually a technique called memes. So this is where you use the same photolithographic patterning techniques, but instead of just leaving the surface as is, you use them as a template for etching the surface away.
And this is what we've done is we've done deep reactive ion etching on actually crystal and silicon. So that's shown here. So this is actually what you build computer chips out of.
We coat them with tissue culture plastic so that we can seed cells on them. And we seed one cell type on one set of these interlocking combs and another cell type on another set of these interlocking combs. And in this set of experiments, what we did is we were able to look at the dynamics of bringing the cells together and apart with micron scale precision.
So using this technique-- I'm just going to summarize here-- this is everything we know about the system to date. And I'm going to go on and tell you how we've used it.
So what we know then is we put two cell types together that existed in a microenvironment in culture and we organize them in different ways, we can alter the emergent tissue function that we get out. So cells are basically dependent on who their neighbors are. And furthermore, there's a temporal component to this rescue.
So if you look at this diagram here what we see is this fat cell with the two nuclei, a hepatocyte, and for the first day or so of culture it's very important that the friendly neighbor is touching it. And after about a day, the friendly neighbor can be further away. So you can imagine you're moving to a new neighborhood. You need friendly neighbors-- you're more dependent on your friendly neighbors in the beginning before you get established.
OK. So we know there's a time component to this rescue. We know there's a shape component to this rescue. I'm not going to tell you about the details today, but we know a lot of molecules that are involved in this rescue. Furthermore, despite the fact that we've identified a lot of molecular players in this system so far none of these alone and none of them in combination can completely replace the effect of having a live cell neighbor. So in all the examples I'm going to show you, we're going to use the living cell neighbor to try and do something useful with these liver tissues.
OK. So now we have a somewhat stabilized hepatocyte of those 500 functions of interest, and I just showed you one that gets rescued, but actually we've looked at very many functions. The next thing that we wanted to do was build an implantable three-dimensional liver.
So I showed you the microarchitecture of the liver. That's actually a very lofty task. And one might start thinking about how one can build complex 3D structures.
So again, if you think about using light and patterns of light to pattern three-dimensional objects, there's a wonderful analog out there in the manufacturing world. This is a process known as stereo lithography. And this is basically a multi-layer version of the process that I've described before.
What you do is you shine light on a pattern on a light sensitive material. You develop the pattern. You wash it away. And in this case, what you then do is deposit another layer, shine light again, and so on and so forth.
So this is a so-called 3D printing process. And these systems are now commercially available. There's many of them around MIT campus. You can just go directly from a CAD drawing to a three-dimensional part.
So we wanted to think about using a technique like this for building living tissues. In order to do that, we needed a light sensitive material that cells would live in. So we chose a hydrogel system called a PEG, a polyethylene glycol hydrogel. It has reactive end groups that are acrylates. It was first developed by Jeff Hubbell. And the way that this works is you mix cells in this liquid, you shine a light on it, and it gets cross-linked, kind of like fruits in jello.
So here are our liver tissues. And this picture, the light has been shown simply in a disc shape so they basically look like soft contact lenses. And what Alice Chen, a graduate student who just defended as shown, is that in these systems, in fact, hepatocytes alone don't function as in the cell culture experiment. If we add those friendly neighbors, they do a little better.
But now that they're in three dimensions, they need a couple of extra things. So here they need some more chemistry from that scaffold. So this is an RGD peptide that binds to a cell surface receptor called an integrin.
And they need other neighbors. So these are the endothelial cells from the liver. So there are two neighboring cell types, some chemistry, and some architecture in this material. And now we can get nice rescue in three-dimensional scaffolds.
So we wanted to then take these in vivo, which I'll show you in a second. But the cool thing about this-- you can roll the movie please. The cool thing about this is-- there you go-- that now because this is a light-sensitive material, we can make all different kinds of shapes of tissues in this multilayer fashion.
So this is a three-layer tissue that we made. This is a kind of tissue that we made where we organized the cells with electric fields before we shone the light to freeze them in place. So now we can look at structure function relationships in three dimensions.
And what you just saw here being made, this is a form of what we call liquid tissue where you're using a microfluidic device to make little droplets of this pre-polymer solution with cells in it and then we shine light on these droplets. And we can just make buckets of these microtissues that you can pipette in, implant in an animal, put in a microfluidic handler.
So because they're light sensitive or very easy to make and then the next thing we like to do is see if we can rescue liver function in a living system. This is my one animal image for the day. This is a mouse that's been implanted with these little contact lenses that have been optimized to have the two friendly neighbors and the right chemistry.
And what you see is this liver has been genetically engineered with a virus so that it expresses an enzyme luciferase that will cause it to glow in the presence of a substrate. So essentially, what you're looking at here is this mouse over time is this little glowing liver over the course of about three months. And it glows better when we implant the livers in the abdomen of the animal, the intraperitoneal site, than we do with just under the skin, the subcutaneous site.
And if we look in the blood of these animals, we can, in fact, see that the human albumin coming from the human livers is present in these animals so we know that the blood stream is hooked up to the liver that we implanted. So this is as far as we've gotten so far. We have little contact lens livers in mice. We have a long way to go.
We need probably about 10 billion cells to get into a human patient. We have lots of ideas about how to scale this up for therapeutic applications. But I wanted to turn to now some sort of nearer-term applications that we're very excited about.
And just to come back to the schematic here, so I've told you about how to make complicated microenvironments with some of these tools. Now, I want to tell you about our interests in interrogating these human liver tissues in vitro, not by implanting them.
So the application, again, that we're interested in is one that I alluded to earlier. And this is a very infamous schematic. This is the drug discovery pipeline.
So it typically takes about 15 years, close to $1 billion, to go from 10,000 small molecules to one FDA-approved drug. And much of the investment in this process happens here in the early years. And this is what we call the pre-clinical phase where you do cell culture experiments, biochemical experiments, and animal experiments before getting into patients.
So one thing that's been disappointing and troublesome for the field is that 8 out of the 9 drugs that get through this pre-clinical phase actually fail once they enter clinical trials. And up to a third of these fail because of drug-induced liver disease. And the main reason for that is the enzymes that detoxify the drugs in your body that I mentioned earlier are exquisitely species specific. So small and large animal models that are required by the FDA simply don't predict well for some of these enzymatic reactions.
OK. So we've been thinking about bridging the gap between animal models and clinical trials with some of these systems that I was describing to you earlier. So this is our new optimized version of the micropattern co-cultures that I showed you earlier, that striped schematic. And this is the organization that's optimal for human cells that allows them to function the longest. And these are those 3D systems that we're also making that are human cells.
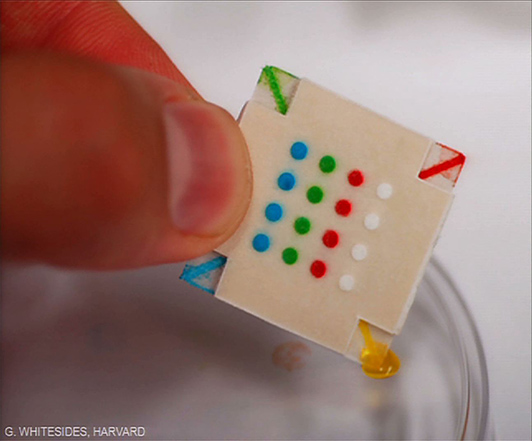
So if we look at this system, we needed to then make this something that pharmaceutical companies could use for looking at libraries of small molecules. So I don't think you'll soon get to 350,000 like Susan was referring to earlier, but something on the order of tens of thousands of compounds. So what we did then was adapt this technology using another relative of photolithography. This is called soft lithography.
And in this technique what you do is you make those same patterns that I described before, but you use them, in fact, to mold polymers. So here what we've done is made stencils out of a polymer called PDMS. And we've put those stencils at the bottom of each well that we wanted to pattern. And in order to pattern it, we pour proteins into the wells and they make sticky spots, and our hepatocytes on those spots, and then we surround them with their friendly neighbors.
And now, what we have is a multi-well plate that looks like the multi-well plates that biologists use routinely that you can dose with drugs and you can do your experiments on. And in fact, you can see that the cells are rescued in this setting as compared to the schematic I showed you before.
So one amazing thing about the MIT community is that we have a real ecosystem here for entrepreneurship. So what we do with this technology was spit out a startup company. And these are data now from the company called Hepregen.
And what's really been exciting for me is as an inventor to see this being now in the hands of real customers that are testing drugs on patients. So this is a historical drug. So it's done in collaboration with Alnylam.
So as I mentioned earlier, only 50% of drugs are predicted correctly and in vitro assays. And one of the main reasons for this is the species-specific metabolism that I mentioned. And also that we all take our drugs every day at low doses.
That's how we take our medicines. But in fact, if you look at the way pharmaceutical drug testing happens it actually happens at 24 hours at high doses. So the mechanisms of toxicity are also different in terms of what one can predict.
So this was a drug. This was a hepatitis B drug. It was an antiviral, [INAUDIBLE]. And in the phase I clinical trial, 5 of 15 patients died within weeks of dosing.
This had not been predicted by rat, dog, or monkey trials. When we went back and put this compound on our human cultures we were able to show that it was toxic and only toxic after multi-day dosing. So we were very excited to see this.
And in particular, now one can go back and look at this compound and look at which parts of the chemical scaffold are actually causing this toxicity so you could redesign a safer version. So this is a historical experiment that we were really excited about using our human microliver platform. But the most exciting thing happened just a month ago. This is unpublished data and I can't name the company so it's called Company X, but the story, I hope, is compelling regardless.
This is a phase I trial for a hepatitis C drug. And it was a combination drug therapy. So what happened in this phase I clinical trial was the patients that were receiving this combination regimen experienced severe elevated liver dysfunction. And the clinical trial was therefore halted by the FDA.
We took these compounds, exposed them chronically to the human microlivers, and it soon became very apparent that one of the compounds was safe and one of the compounds was toxic. We went and used that data, went back to the FDA, and asked to restart the clinical trial with the apparently safe compound in combination with the existing standard of care. And the FDA said yes.
So starting this fall, the new clinical trial will be designed using the data from our platform. So this was, as I said, a real thrill as an inventor.
So I've told you about how we're building implantable livers. I told you about how we're interrogating miniaturized human microlivers. And I just want to give you a glimpse of one thing that we're really excited about, a direction that we're going. And that is trying to learn more about how the liver interacts with infections.
So I mentioned earlier that hepatitis A, B, and C, all the hepatides are actually viral infections of the liver. But one thing you might not realize is that malaria is also an infection of the liver. So what I'm showing you here is the malaria lifecycle.
This is a mosquito biting a person and this parasite going into the bloodstream. The first place it infects, actually, is the hepatocyte, the liver. And there it expands, it amplifies many, many times. It undergoes morphogenesis, and it bursts out into the blood.
When it infects red blood cells, that's when you get the characteristic symptoms of malaria that we all know, the fever. So many groups have been interested in treating malaria at the liver stage because you start with something like 30 sporozoites and you end up with about 300,000 in the blood. So there's a huge amplification. And if you could treat it at the liver stage that would be ideal.
It turns out there are no good in vitro models of the human liver infection of these malaria organisms. And therefore, there are no good drug screening models for liver stage infection. In particular, we're really interested in this particular kind of malaria, Plasmodium vivax, which actually has a hibernating form where it hibernates in the liver. No one has seen in vitro this hibernating form of Plasmodium vivax.
It's called the hypnozoite because it's hypnotized. And it takes about three weeks to hibernate. And so now that our livers live for about 4 to 6 weeks, we're really excited about the potential to get a glimpse of this organism to get drugs against it.
Roll the movie please. This is my last movie. There we go.
So this is a sporozoite gliding in one of our cultures. This is a parasite that's been dissected from the salivary gland of a mosquito in our laboratory and now put on one of our human microlivers. And the cool thing about this parasite is actually it can sample many hepatocytes on the way to picking the one that it will grow in. So what you're looking at here is all the hepatocytes that it's wounded in our culture as it's invading.
And we can see now for the first three hours that once it gets inside that it's adopting some of those morphogenetic forms. So I'm not going to show you all the data today, but we've now fully recapitulated the liver stage lifecycle of both Plasmodium falciparum and Plasmodium vivax. And with Gates Foundation funding we're now doing a drug screen at the Broad to pursue some of these new therapeutics.
So just to summarize and to wrap everything together, what I've told you about is our interest is in how cells interact in communities and how we can use some of these tiny technologies that are assembled here for constructing healthy microenvironments, for interrogating microenvironments, and for studying the interaction of these microenvironments with pathogens like infections. And we've been using this approach not just to build healthy liver environments, but also to try and treat cancer microenvironments, which I won't have time to tell you about today.
Ultimately, we think these microenvironments impact the health of the organism and, of course, the health of society. I want to just spend the last few minutes for any young people that might be out there to say the following, which is that this has just been a fabulous place to do science. And in case you think it's a solitary profession, it's absolutely not. This is my microenvironment. This is my team.
These are the graduate students and post-docs and staff and undergraduates in the laboratory. This hardy bunch moved from California where it used to be at UC San Diego here by the beach to MIT to join in the vibrancy of this environment. And I want to say too that another thing that I'm really grateful for is that we don't work all the time. So I spend lots of non-scientific time with my husband and daughters and parents and girlfriends from college. And I'm really thankful for that too.
And finally, we here at MIT are trying to pay forward the gifts that we've been given. So through the Society of Women Engineers, there's actually an outreach activity that many of you may have heard of. These are Saturday afternoon workshops for middle school girls, which have been identified to be some of the bigger ages for risk for losing interest in science and engineering. And here they are just so heartwarming for me to see just filling up our lab.
Here this young girl. She's 11 years old holding her first microfluidic device. So hopefully, she'll be spreading the word. So thank you so much for your attention and I'm happy to take questions.
[APPLAUSE]
MODERATOR: Any questions?
AUDIENCE: You mentioned scaling up. Can you say something about what would be required to go from the scaffolding you have to a block of cells that would actually keep growing into a full organ?
BHATIA: Sure. So there's two components. Obviously, there's the growth of the cells and there's the architecture. So one idea we've been exploring is to take those liquid microtissues, those 200 micron pieces of microtissue, and thinking about ways to assemble them, to self-assemble them, into larger structures. So [? Sherry ?] [? Lee is ?] a chemical engineering student in our group who's been templating surfaces to start off that self-assembly and to drive the self-assembly actually via DNA codes to try and make larger and larger structures.
So that's one piece of it. That's assembling the scaffold. The other piece is getting enough cells.
So it turns out there's this paradox in the liver literature, which is that hepatocytes grow in your body. Liver generation is not a stem cell-driven process. It's actually the mature hepatocyte that can grow. And so we've actually just completed a screen at the Broad Institute where we've identified some molecules to make hepatocytes grow. And so we hope that we'll have enough cells and enough self-organizing scaffolds to make these bigger structures.
AUDIENCE: This is actually more of a comment, but I loved your talk and it's very interesting. But in addition, it seems like in a biological sense what you discovered is-- and you discovered how to do it, but critical mass. That just a couple of liver cells isn't going to do it. You have to organize them into a critical mass that can act coherently, and that's what we were talking about before. So that was a great rounding back, even if you didn't mean it.
BHATIA: Yeah. Well, thank you for the extension of the analogy. I totally agree.
AUDIENCE: Hi. I was wondering in your drug screening assays, what is the primary method of determining whether it's toxic to the human liver cells that are in your cultures?
BHATIA: Yeah. That's a great question. So actually there are several readouts that folks will use.
So one is just ATP depletion and the other will be mitochondrial activity. The third could be mitochondrial potential. The fourth could be reactive ion species. So there are these panels of metrics that folks use. And typically, every company has their own favorite way.
We're interested in doing multiparametric testing now with high content imaging. So we measure membrane integrity, ATP levels, and mitochondrial potential more routinely. Mhm? OK, great.
MODERATOR: OK. Thank you. Fantastic.
[APPLAUSE]
MODERATOR: Well, I'd like to Sangeeta for a really, really exciting talk. And I'd like to thank our three speakers for the session for really truly outstanding talks and for sharing their groundbreaking research with us today.
[APPLAUSE]